Cuando existe un trastorno psicológico se requiere, a fin de superarlo, que la persona que lo padece quiera mejorarlo o eliminarlo para siempre. Esta afirmación puede parecer un contrasentido ya que nadie desea sufrir gratuitamente; sin embargo, no es así de sencillo ya que la superación requiere un esfuerzo, a veces muy intenso, de quién lo sufre. Y ahí viene el dilema. “¿Merecerá la pena todo el esfuerzo y la lucha que se ha de realizar para desterrar ese mal que está afectando de continuo a la persona?” La respuesta dependerá de la motivación que tenga.
¿Qué es lo que motiva a una persona a hacer algo?
Existen motivaciones internas no conocidas por las personas que las poseen. Estas son las motivaciones llamadas inconscientes. La motivación se puede entender como un conjunto de factores que determinan un comportamiento. En definitiva, es el ensayo mental preparatorio de una acción.
Los motivos no son siempre objetivos y por tanto no son comunes a todos; no tienen el mismo origen, ni la misma intensidad, no todos tenemos el mismo sistema de valores. Lo que uno valora en una escala numérica del cero al diez, con un nueve, hay otro que ese valor lo cuantifica con un uno o ni siquiera lo valora. Es por ello, por lo que cada persona tiene que encontrar su razón realmente motivadora que le conduzca a ponerse en marcha.
Caso clínico a modo de ejemplo.
Se trataba de un hombre extranjero de alrededor de cuarenta años, que empezó un tratamiento psicológico por un problema de alcoholismo. Tenía problemas en el trabajo; con su mujer e hijos a los que veía sufrir constantemente; con su salud, ya muy deteriorada hasta el punto de padecer una hepatitis crónica; estados de depresión continuos y en definitiva, la carencia de una mínima calidad de vida.  Él era consciente de que la solución era solamente una: dejar de beber. ¿Pero como conseguirlo? Manifestaba: -“quiero a mi mujer, adoro a mis hijos, valoro mi salud, me gusta mi profesión… y aún sumando todos ellos, no tengo fuerza para plantearme definitivamente ese BASTA YA, que es lo único que debo hacer”
Él era consciente de que la solución era solamente una: dejar de beber. ¿Pero como conseguirlo? Manifestaba: -“quiero a mi mujer, adoro a mis hijos, valoro mi salud, me gusta mi profesión… y aún sumando todos ellos, no tengo fuerza para plantearme definitivamente ese BASTA YA, que es lo único que debo hacer”
 Él era consciente de que la solución era solamente una: dejar de beber. ¿Pero como conseguirlo? Manifestaba: -“quiero a mi mujer, adoro a mis hijos, valoro mi salud, me gusta mi profesión… y aún sumando todos ellos, no tengo fuerza para plantearme definitivamente ese BASTA YA, que es lo único que debo hacer”
Él era consciente de que la solución era solamente una: dejar de beber. ¿Pero como conseguirlo? Manifestaba: -“quiero a mi mujer, adoro a mis hijos, valoro mi salud, me gusta mi profesión… y aún sumando todos ellos, no tengo fuerza para plantearme definitivamente ese BASTA YA, que es lo único que debo hacer”
Cuando estos casos se presentan en un tratamiento psicológico, no sólo en el alcoholismo sino en cualquier otro trastorno psicológico del tipo que sea, como puede ser un trastorno obsesivo, dismorfofobia, ludopatía, trastornos alimentarios etc. se debe ayudar al paciente a encontrar la motivación, “su motivación” a fin de que se disponga a luchar para superar su problema.
Volviendo al caso anterior, era evidente que ni la salud, ni el trabajo, ni la familia, ni la suma de esos componentes eran suficiente motivo para comenzar la lucha contra el alcohol. Bastó con encontrar la motivación que este paciente necesitaba para impulsarle a la acción. En su caso fue el ayudar a compatriotas suyos. Había un grupo desasistido en aquel entonces que por falta de unión, medios y problemas con el idioma, presentaba muchísimas carencias. Este paciente sintió el ímpetu, la llamada y el coraje para plantearse ese “BASTA YA” y con ayuda del tratamiento, erradicar el alcohol de su vida, uniéndose a sus paisanos y prestándoles toda su ayuda.
Como decíamos anteriormente, no sólo en los casos de adicciones se ha de encontrar la motivación adecuada para emprender la lucha. En las obsesiones se necesita para vencer las compulsiones. En la agorafobia para eliminar las conductas de evitación. En la fobia social para enfrentarse a aquellas situaciones que la persona considera imposibles de superar. En definitiva, para la superación de cualquier tipo de trastorno psicológico o situación trágica y penosa que en la vida se presente, siempre se requiere un esfuerzo de la persona que lo padece.
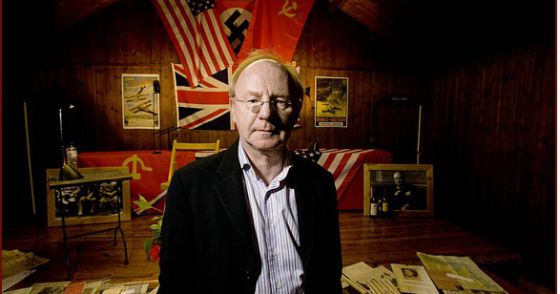
¡Que bien lo entendió Victor Frankl!, cuando a través de su motivación y de buscar su sentido de vida, pudo superar las atrocidades del campo de concentración donde estuvo prisionero. Allí escribió “El hombre en busca de sentido”, que le sirvió de motivación para sobrevivir. Su motivo, su sentido de vida, fue la ayuda a los demás.
La motivación es lo que nos mueve desde dentro. Cada persona debe encontrar sus propios motivos, su propio trampolín que le ayude a tomar impulso y a luchar contra sus adversidades.